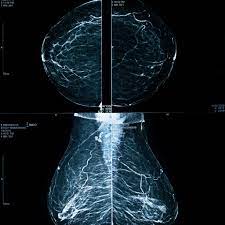
Harms of Breast Cancer Screening: Systematic Review to Update the 2009 U.S. Preventive Services Task Force Recommendation
In 2009, the U.S. Preventive Services Task Force recommended biennial mammography screening for women aged 50 to 74 years and selective screening for those aged 40 to 49 years.
Purpose:
To review studies of screening in average-risk women with mammography, magnetic resonance imaging, or ultrasonography that reported on fals+
positive results, overdiagnosis, anxiety, pain, and radiation exposure.
Data Sources:
MEDLINE and Cochrane databases through December 2014.
Study Selection:
English-language systematic reviews, randomized trials, and observational studies of screening.
Data Extraction:
Investigators extracted and confirmed data from studies and dual-rated study quality. Discrepancies were resolved through consensus.
Data Synthesis:
Based on 2 studies of U.S. data, 10-year cumulative rates of false-positive mammography results and biopsies were higher with annual than biennial screening (61% vs. 42% and 7% vs. 5%, respectively) and for women aged 40 to 49 years, those with dense breasts, and those using combination hormone therapy. Twenty-nine studies using different methods reported overdiagnosis rates of 0% to 54%; rates from randomized trials were 11% to 22%. Women with false-positive results reported more anxiety, distress, and breast cancer–specific worry, although results varied across 80 observational studies. Thirty-nine observational studies indicated that some women reported pain during mammography (1% to 77%); of these, 11% to 46% declined future screening. Models estimated 2 to 11 screening-related deaths from radiation-induced cancer per 100 000 women using digital mammography, depending on age and screening interval. Five observational studies of tomosynthesis and mammography indicated increased biopsies but reduced recalls compared with mammography alone.

The harms of mammography include the following:
False-positive test results can occur.
Screening test results may appear to be abnormal even though no cancer is present. A false-positive test result (one that shows there is cancer when there really isn’t) is usually followed by more tests (such as biopsy), which also have risks.
When a breast biopsy result is abnormal, getting a second opinion from a different pathologist may confirm a correct breast cancer diagnosis.
Most abnormal test results turn out not to be cancer. False-positive results are more common in the following:
- Younger women (under age 50).
- Women who have had previous breast biopsies.
- Women with a family history of breast cancer.
- Women who take hormones for menopause.
False-positive results are more likely the first time screening mammography is done than with later screenings. For every ten women who have a single mammogram, one will have a false-positive result. The chance of having a false-positive result goes up the more mammograms a woman has. Comparing a current mammogram with a past mammogram lowers the risk of a false-positive result.
The skill of the radiologist also can affect the chance of a false-positive result.
False-positive results can lead to extra testing and cause anxiety.
If a mammogram is abnormal, more tests may be done to diagnose cancer. Women can become anxious during the diagnostic testing. Even if it is a false-positive test and cancer is not diagnosed, the result can lead to anxiety anywhere from a few days to years later.
Several studies show that women who feel anxiety after false-positive test results are more likely to schedule regular breast screening exams in the future.
False-negative test results can delay diagnosis and treatment.
Screening test results may appear to be normal even though breast cancer is present. This is called a false-negative test result. A woman who has a false-negative test result may delay seeking medical care even if she has symptoms. About one in 5 cancers are missed by mammography.
The chance of a false-negative test result is more common in women who:
- Are younger.
- Have dense breast tissue.
- Have cancer that is not dependent on hormones (estrogen and progesterone).
- Have cancer that is fast growing.
Finding breast cancer may lead to breast cancer treatment and side effects, but it may not improve a woman’s health or help her live longer.
Some breast cancers found only by screening mammography may never cause health problems or become life-threatening. Finding these cancers is called overdiagnosis. When these cancers are found, having treatment may cause serious side effects and may not lead to a longer, healthier life.
Mammography exposes the breast to low doses of radiation.
Being exposed to high radiation doses is a risk factor for breast cancer. The radiation dose with a mammogram is very low. Women who start getting mammograms after age 50 have very little risk that the overall exposure to radiation from mammograms throughout their lives will cause harm. Women with large breasts or with breast implants may be exposed to slightly higher radiation doses during screening mammography.
There may be pain or x-ray discomfort during a mammogram.
During a mammogram, the breast is placed between two plates that are pressed together. Pressing the breast helps to get a better of the breast. Some women have pain or discomfort during a mammogram. The amount of pain may also depend on the following:
- The phase of the woman’s menstrual cycle.
- The woman’s anxiety level.

Limitations:
Studies of overdiagnosis were highly heterogeneous, and estimates varied depending on the analytic approach. Studies of anxiety and pain used different outcome measures. Radiation exposure was based on models.
Conclusion:
False-positive results are common and are higher for annual screening, younger women, and women with dense breasts. Although overdiagnosis, anxiety, pain, and radiation exposure may cause harm, their effects on individual women are difficult to estimate and vary widely.
